Employee Engagement in NHS Healthcare
Deploying collaborative technologies to drive better staff engagement and improve patient outcomes
The UK healthcare system is defined by one key element: it’s people.
Engaging those at the frontline of the NHS to be dedicated, committed and evolved with their roles is key to its success. David Astley O.B.E., a former NHS Trust CEO, summoned it up simply: “happy staff make for happy patients”.
The body of evidence showing that engaged staff deliver better care is growing; engaged staff equate to lower mortality rates, higher patient satisfaction levels and stronger financial performance, to name a few. And the list doesn’t stop there.
However, the challenge of how to create this seemingly mythological ‘engaged employee’ remains.
Despite tools, resources and research into the topic, the annual NHS Staff Survey shows there are discrepancies in engagement levels between trust types and geographical regions. Engagement, as the NHS defines it, is increasing year-on-year; but slowly, and disparately.
Practical support and advice for those charged with transforming engagement levels spans a vast range of topics, including leadership models, staff appraisals and more. We explore the increasingly vital role technology plays in shaping employee experience.
Defining employee engagement within the NHS
Employee engagement is far from new as a concept, with many definitions existing across the web. Custom Insight explains:
“Employee engagement is the extent to which employees feel passionate about their jobs, are committed to the organization, and put discretionary effort into their work.”
More explicitly still, MacLeod and Clarke (2009) identify the core element of engagement as the relationship; “it is when the business values the employee and the employee values the business.”
Simply, employee engagement is not the sole responsibility of either employee or employer: it is about the relationship between the two.
When it comes to the UK healthcare system, the concept of employee engagement goes further. In fact, it is alluded to within elements of the NHS constitution, which pledges to;
“Engage staff in decisions that affect them and services they provide […] All staff will be empowered to put forward ways to deliver better and safer services for patients and their families.”
“Provide a positive working environment for staff and to promote supportive, open cultures that help staff do their job to the best of their ability”
Measurement of engagement within the NHS is undertaken through the annual NHS Staff Survey, which introduced the element in 2009. It defines engagement across 3 dimensions:
- Psychological: whether staff look forward to coming to work, feel enthusiastic about their role and feel that time passes quickly when they are in work
- Advocacy: if staff would recommend their organization as a place to work and be treated
- Involvement: the extent to which staff feel they can put forward suggestions for improvement, have opportunities to show initiative and can drive improvements
Fundamentally, all definitions share a common theme: they discuss the ways in which people behave when they are engaged. Buzzwords span from “energetic”, “determined” and “enthusiastic” through to “inspired” or “dedicated”. Staff will go above and beyond their core roles and give more to their organization.
The result is a definition that can be aligned with measurable, tangible outcomes – in the case of the NHS, in terms of mortality rates, staff absence or turnover rates, patient feedback or financial returns.
In “The Evidence” report into employee engagement, Professor Mike West of the Centre for Performance-led HR at Lancaster University concluded, “Employee engagement emerges as the best predictor or NHS trust outcomes.”
The value of employee engagement for healthcare providers
On its Staff Engagement page, the NHS Employers site emphasizes the role of engagement in supporting the NHS to meet the range of challenges it currently faces.
With GBP22billion of efficiency savings to be achieved my 2021 as the NHS continues to action guidance outlined in the Five Year Forward View, change is extensive and ongoing. Ensuring the support and continued investment of staff into that process is paramount.
However, what is the value at trust level of increased employee engagement?
Research by The King’s Fund and West and Dawson (2012), amongst others, point to many organizational performance outcomes linked to employee engagement:
- Better patient experience
- Fewer medical errors
- Lower infection and mortality rates
- Stronger financial management
- Higher staff morale and motivation
- Less absenteeism, stress and incidences of burnout
- Increased staff retention
- Improved staff experience and productivity
Specific gains are outlined in the NHS Staff Engagement toolkit, covering gains not only at patient and trust performance level, but at employee level also;
On the other end of the scale, the costs of poor engagement can be extensive.
As a public body, the NHS faces unique challenges when it comes to change and decision-making. In its examination into the hospital chain model, PwC observed:
“Recent high-profile top-down reorganisation efforts have left frontline NHS care professionals disillusioned and increasingly fatigued by imposed change”
The feeling of powerlessness and ‘not having a voice’ by on the ground staff may be one of the triggers for this year’s strike action over junior doctor contracts; a series of protests that sparked nationwide discussion and media attention. Observing the turn of events, former health minister Dr Poulter argued that morale stands at the “lowest point” the NHS has ever seen – putting patients at risk.
The cost of absence and staff turnover – not only in terms of deploying agency staff or in recruitment and training costs, but in lost productivity and its knock-on implications for patient care – is also significant.
By improving sickness absence by just 1%, the NHS will recuperate GBP280m in staff costs
(Source: ‘Operational productivity and performance in English NHS acute hospitals: Unwarranted variations’, Lord Carter)
Considering the business case for engagement, it is widely recognised by NHS trusts throughout the UK that this is no longer as no longer a ‘nice to have’: but a fundamental part of long-term trust strategy.
Driving staff engagement in the NHS
In its paper, ‘Staff engagement: Six building blocks for harnessing the creativity and enthusiasm of NHS staff’, The King’s Fund point to the following elements required to drive engagement:
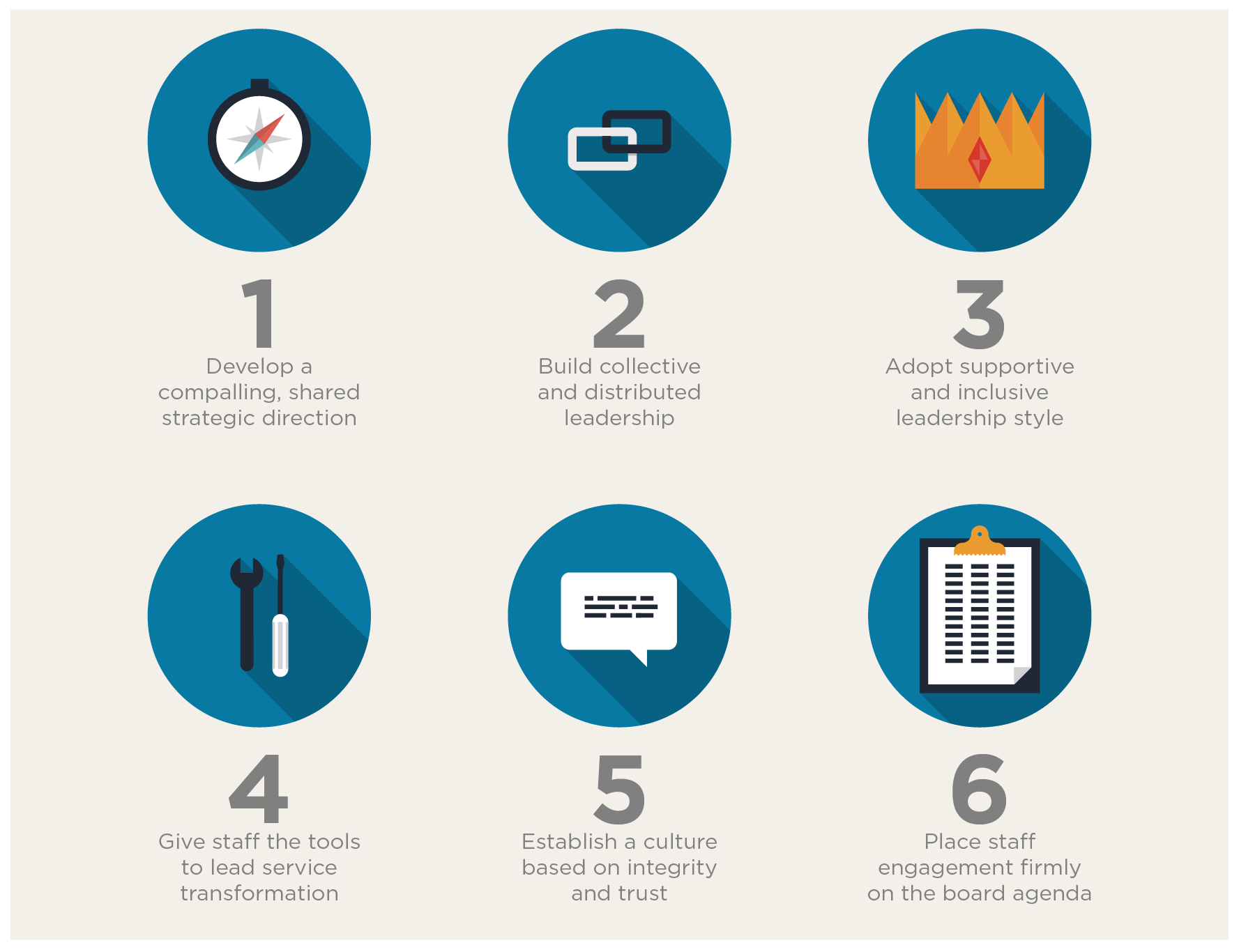
One of the biggest areas of focus for advisors to the NHS is that of shifting from historic models of “heroic individual” leaders, and towards a shared and distributed method of leadership – a process of collaborative management. There is also importance assigned to staff involvement in the decision-making process, including the empowerment of staff to communicate with management.
Engagement, therefore, calls for a different approach, The King’s Fund paper argues;
“It emphasises teamwork, collaboration and ‘connectedness’, and removes barriers to communication and original thinking”.
In a historically inflexible, top-down infrastructure typically seen within the NHS, facilitating this approach is a challenge.
How can NHS leaders work in partnership outside of established silos and across boundaries, developing supportive relationships? How can they empower staff by taking on board their concerns and perspectives, while showing they are actioning their ideas?
Collaborative technology can – and should – play a central role.
Deploying technology to support staff engagement in the NHS
Collaborative technologies are increasingly recognised for their contributory role in building internal cultures and facilitating communication. In line with the recommendations of the ‘Six building blocks’ outlined by The King’s Trust, we explore how technology can support the specific engagement goals of the NHS.
1. Develop a compelling, shared strategic direction
A clear vision and organisational narrative can support staff in feeling connected to their roles and the overarching direction of their organisation. Creating and communicating the strategic mission of any trust helps staff feel a sense of purpose – furthering their sense of engagement.
It stands to measure that top-performing NHS organisations, therefore, must be mission-driven. Using a collaboration platform to establish, communicate and then embed strategic direction and purpose can prove hugely beneficial.
By enabling cross-organizational conversations, management can obtain feedback from staff outside of management silos. Staff surveys, polls and interactions via blogs or social tools empower staff to provide feedback and help defining company vision: a shared vision, from ward to board.
“Leaders need to demonstrate their commitment to the vision through the way they spend their time, how they allocate resources, what they measure and what they reward, as well as by ensuring that the vision is reflected in staff objectives across the organisation.” (The King’s Fund)
Communicating and embedding strategic direction, business vision and values needs to be facilitated on a regular basis, across all members of staff: whether they work in hospitals, out in the community or remotely.
Utilising a staff intranet to keep employees informed about accomplishments or actions aligned to your strategic mission can help build engagement and ensure staff feel connected.
2. Build collective and distributed leadership / Adopt supportive and inclusive leadership styles
The changes demanded of leadership and management structures within the NHS all have a similar theme: they emphasise collaborative practices, going beyond the individual.
“Leadership [needs to] act as a ‘cognitive catalyst’. Gone is the heroic individual with a monopoly on the vision; it is replaced by a commitment to building shared visions with a range of stakeholders. It exploits the diversity of perspectives and the wealth of experiences, strengths and potential in the organisation. It’s teamwork.” (Source: ‘Leadership and Engagement for Improvement in the NHS’, The King’s Trust)
Due to the dispersed structure of many trusts, building a collective leadership that brings together representatives from across its distributed functions presents a logistical hurdle.
With collaborative technologies, individuals can connect regardless of department or location. An intranet with forums, team functionality and blogs offers an ideal platform for idea exchange or sharing of best practice; a way to develop leadership models that adopt successful strategies from across multiple individuals or even trusts. It can help build connections and facilitate conversations.
What’s more, those in leadership roles can act upon the building block of inclusivity and support by using collaborative technologies to communicate with their people.
By giving staff the tools they need to voice their concerns and providing visibility of board-level strategy, they can promote a different type of leadership: one that listens, engages, and empowers employees, putting them first. This can help address fears by some that transformational management could overstep into intimidation – ensuring balance.
In this TEDTalk, Vineet Nayar recounts his personal experience as CEO of defying the conventional wisdom that companies must put customers first, when he decided to turn the hierarchical pyramid upside down by making management accountable to the employees, and not the other way around.
3. Give staff the tools to lead service transformation
In the public sector, the ability to exercise control and authority over both individual roles and the organisation can be limited.
Empowering staff to drive change, however, is directly linked to levels of engagement. As the ‘on the ground’ representatives of the NHS, these are also arguably the best positioned staff to identify areas for improvement – and action them.
Devolving responsibility for service transformation to those on the frontline is now becoming increasingly popular throughout trusts. Giving staff a voice and involving them in change initiatives can be supported by collaboration and communication tools.
Social tools such as blogs, forums, comment functionality and polls all enable your employees to provide feedback and insight. When service transformation initiatives are agreed, new practices need to be communicated using management blogs or via new policy documents, giving staff what they need to ensure buy-in and then to action changes.
A collaborative platform such as an intranet also allows staff to connect to share best practice, learn from others successes and seek help and advice from the collected knowledge pool residing within their organisation.
4. Establish a culture based on integrity and trust
Establishing internal cultures across different departments or disciplines, remote or mobile workers and multiple sites is a challenge for any NHS organisation.
Some staff will never meet face-to-face; others will never have visibility of operations or the achievements of others. Trusts must establish mobile cultures without walls. However, creating a culture of integrity and trust without that ‘connectedness’ is difficult.
Business cultures are complex, built upon many elements. However, they can be supported and embedded by a strong internal brand and internal communications strategy.
This follows directly from point 1: establishing a mission and values, which underpin any culture, is key. Collaborative platforms can be used to communicate and align successes to those, demonstrating integrity to the fundamental drivers of your organisation and ensuring transparency – across all employees.
If your mission is to have the highest patient rating of any trust, for example, a healthcare intranet can be used to inform and educate staff on how to achieve this. Success can be celebrated; mistakes learned from. Policies and compliance to achieve goals can be hosted, easily accessible and visible.
Open, two-way communication and demonstrating that staff have been heard and their points actioned will embed trust. In these instances, the value of digital collaboration tools can’t be underestimated.
5. Place staff engagement firmly on the board agenda
Improving staff engagement is embedded into the NHS constitution and a primary focus of research and discussion about the future of the UK healthcare system. Now, it’s time to bring it onto the individual trust board agenda. However, it’s clear retention and engagement strategy is still not universally considered a priority, as HR representatives reported.
Beyond the NHS annual Staff Survey, individual trusts must benchmark and assess employee engagement levels within their own organisations. However, as a largely ‘soft’ outcome, engagement is notoriously difficult to measure.
A digital collaboration platform such as an intranet provides unique access to analytics and usage statistics that can be used to identify what staff are searching for, how often they access different areas of the online community and contribute, and provide feedback on the receptiveness to specific initiatives or policies.
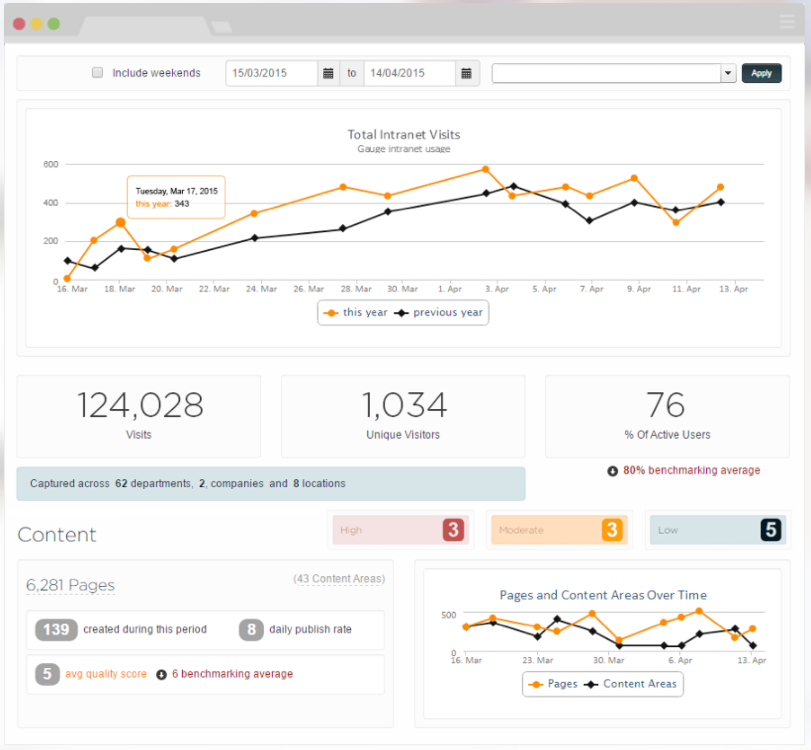
Enterprise search functionality can also be used to pull up conversations, providing on-the-ground insight usually inaccessible to board management. Polls, Q & A forums and other sources of two-way conversation within a collaboration platform ensure the concerns of staff remain front of mind – trying employee engagement off the hospital ward and into the boardroom.
Employee engagement and technology: a partnership
Employee engagement has proven rewards, both within and external to the healthcare system.
For those Trusts who action it as a priority, higher levels of engagement can ultimately lead to increased retention, reduced sickness and absence rates, higher patient care and satisfaction levels and improved financial performance. In building, benchmarking and responding to employee engagement goals, technology must play a central role.
Do you have an online community or collaboration platform within your trust? Have you noticed differences in employee engagement or buy-in? What measures do you have in place to benchmark and improve levels of engagement? We’d love to hear from you – leave us a comment!